Mammograms can find cancer early before symptoms appear. Regular screening decreases the risk of dying from breast cancer. But a recent survey question by the Annenberg Public Policy Center shows that some Americans appear to be confused about when women with an average risk of breast cancer should begin a regimen of regular mammograms.
Women with an average risk of breast cancer should begin to have mammograms every other year beginning at age 40, according to the U.S. Preventive Services Task Force, which issued an updated recommendation on April 30, 2024, in the Journal of the American Medical Association, formalizing an earlier draft proposal. The recommendation applies to women from ages 40 to 74.
Founded in 1984, the U.S. Preventive Services Task Force is “an independent, volunteer panel of national experts in prevention and evidence-based medicine.” It offers guidance to federal health agencies and, through the Affordable Care Act, essentially determines which preventive services should be covered by insurers.
Guidance from major medical organizations on what age to begin regular mammograms has changed over the years – from 40 to 50 and then back to 40 again. While a start date of age 40 is widely recommended, some medical organizations have put forth other recommendations. The American Cancer Society, for instance, advises that women with average risk have the option to start screening every year from age 40 to 44, then should have mammograms annually from 45 to 54 years old, and then continue with mammograms every other year.
The Annenberg Public Policy Center (APPC)’s health survey, conducted with a sample of over 1,600 U.S. adults in April, finds that nearly half of those surveyed (49%) know that age 40 is when women at an average risk of breast cancer should begin to have mammograms every other year. But 10% say they should begin at age 20; 21% say age 30; 8% age 50; and 11% are not sure.
“Confusion can arise when medical guidance about detection or treatment changes, as it has in recent years with mammograms,” said Kathleen Hall Jamieson, director of the Annenberg Public Policy Center of the University of Pennsylvania. “Our data suggest that the recommendation that such screening ordinarily start at 40 years old is not yet widely enough known.”
In our April 2024 survey, conducted before the task force lowered its recommendation from age 50 to age 40, the overall finding was the same: 49% thought the correct age was 40. That was not the recommended age at that time, though it is today with the updated medical advice.
More uncertainty among younger women
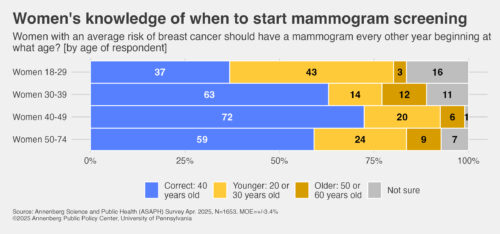
Among the women surveyed, nearly three-quarters (72%) who are ages 40-49 years old know that regular mammograms should begin at age 40. About 6 in 10 women age 30-39 years old (63%) and 50-74 years old (59%) know this as well (the percentage difference between them is not statistically significant). Younger women are the least well-informed about when to begin mammograms – among women 18-29 years old, just over a third (37%) know the correct age.
In addition, more younger women say they are not sure what the correct age is. The survey finds that 16% of women 18-29 years old and 11% of women 30-39 years old are not sure at what age to begin having mammograms. There is no statistically significant difference between those two age groups – but both differ significantly from the very small percentage of women 40-49 years (1%) who are not sure of the age to being having mammograms.
Among 18- to 29-year-old women, the most commonly selected incorrect age for when to begin regular mammography is 30 years old (selected by 27%) – a decade earlier than recommended. Among women 30-39 years old, those who are approaching the recommended start age for mammograms of 40 years old, the most commonly selected incorrect age is 50 years old (selected by 12%) – a decade later than current recommendations.
APPC’s Annenberg Science and Public Health survey
The survey data come from the 24th wave of a nationally representative panel of 1,653 U.S. adults conducted for the Annenberg Public Policy Center by SSRS, an independent market research company. Most have been empaneled since April 2021. To account for attrition, replenishment samples have been added over time using a random probability sampling design. The most recent replenishment, in September 2024, added 360 respondents to the sample. This wave of the Annenberg Science and Public Health (ASAPH) survey was fielded April 15-28, 2025. The margin of sampling error (MOE) is ± 3.4 percentage points at the 95% confidence level. All figures are rounded to the nearest whole number and may not add to 100%. Combined subcategories may not add to totals in the topline and text due to rounding.
Download the topline and the methods report.
The policy center has been tracking the American public’s knowledge, beliefs, and behaviors regarding vaccination, Covid-19, flu, RSV, and other consequential health issues through this survey panel for four years. APPC’s ASAPH team consists of research analyst Laura A. Gibson; Patrick E. Jamieson, director of the Annenberg Health and Risk Communication Institute; and Ken Winneg, managing director of survey research.
See other recent Annenberg health survey news releases:
- High blood pressure: Many Americans unaware high blood pressure usually has no noticeable symptoms (June 6, 2025)
- Measles and the MMR vaccine: Americans say benefits of MMR vaccine for children outweigh risks by nearly 5-1 (May 16, 2025)
- Raw milk and bird flu: With bird flu in raw milk, many still do not know risks of consuming it (March 14, 2025)
- Firearm safety: Over 1 in 3 adults in households with guns do not store all in locked locations (March 11, 2025)
- Low-dose aspirin: Nearly half of adults mistakenly think benefits of daily aspirin outweigh risks (Feb. 3, 2025)
The Annenberg Public Policy Center was established in 1993 to educate the public and policy makers about communication’s role in advancing public understanding of political, science, and health issues at the local, state, and federal levels. Connect with us on Facebook, X, Instagram, and Bluesky.